Mental health and substance abuse often intersect, casting long shadows over the lives of individuals and their families. These twin challenges are deeply intertwined, as mental health issues can drive substance use and, conversely, substance abuse can exacerbate or trigger mental health problems. This blog aims to shed light on this complex relationship, offering insights into the underlying causes, the impacts, and most importantly, the paths to recovery and support.
Contents
How Mental Health And Substance Abuse Are Related?
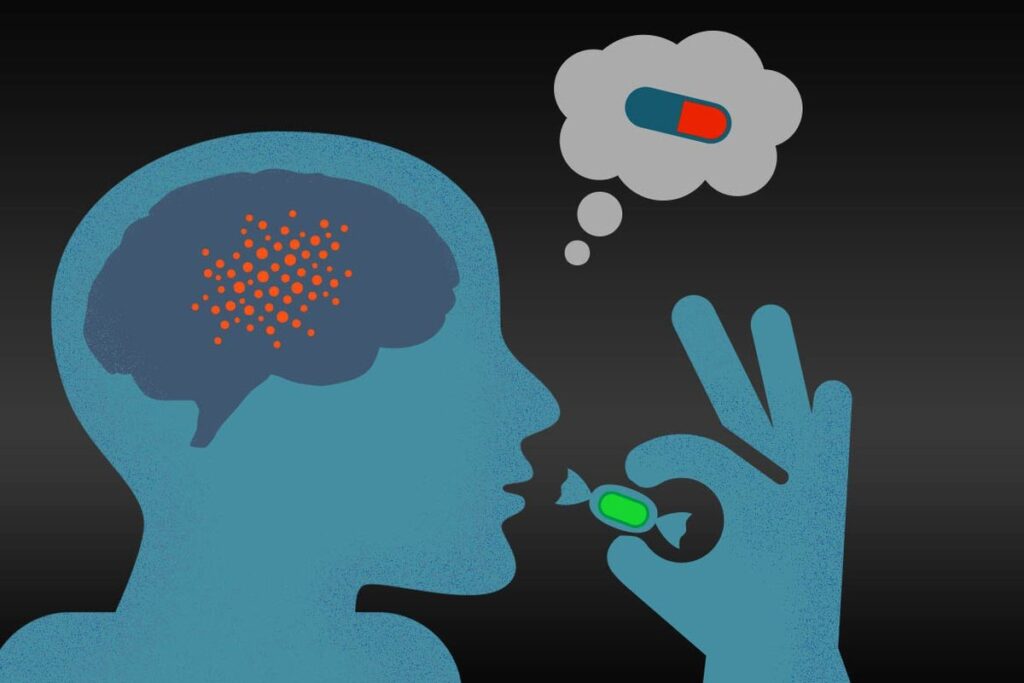
 Mental health issues and substance abuse are often closely linked in what health professionals refer to as dual diagnosis or co-occurring disorders. This relationship can manifest in a cyclical nature—mental health problems can precipitate substance use as individuals attempt to self-medicate and alleviate the symptoms of disorders such as depression, anxiety, or schizophrenia.
Mental health issues and substance abuse are often closely linked in what health professionals refer to as dual diagnosis or co-occurring disorders. This relationship can manifest in a cyclical nature—mental health problems can precipitate substance use as individuals attempt to self-medicate and alleviate the symptoms of disorders such as depression, anxiety, or schizophrenia.
Conversely, the abuse of substances can exacerbate or trigger the onset of mental health disorders by altering brain chemistry. This can lead to changes in mood, perception, and behavior.
The dynamics of this relationship are complex and influenced by various factors including genetics, environment, and individual psychology. For instance, someone with a family history of mental health issues may be more susceptible to developing similar problems, and substance abuse can increase that risk.
Co-occurring Substance Abuse Mental Health Conditions
Co-occurring substance abuse and mental health conditions involve the simultaneous presence of a mental health disorder and a substance use disorder. Here are some of the most common conditions:
- Depression: Many individuals with depression may turn to alcohol or drugs as a way to escape their feelings of sadness or emptiness, but substance use can worsen depressive symptoms over time.
- Anxiety Disorders: This includes generalized anxiety disorder, panic disorder, and social anxiety disorder, where individuals might use substances to alleviate their intense feelings of anxiety or fear.
- Bipolar Disorder: Characterized by dramatic shifts in mood, energy, and activity levels, individuals with bipolar disorder may misuse substances during manic episodes as part of impulsive behavior or during depressive episodes to feel better.
- Post-Traumatic Stress Disorder (PTSD): People with PTSD often struggle with intense and disturbing thoughts and feelings related to their experiences. They might use substances to numb their emotional pain or to cope with insomnia and nightmares.
- Schizophrenia: Substance use among individuals with schizophrenia is common, often exacerbating symptoms like hallucinations and paranoia but sometimes used in an attempt to alleviate these distressing symptoms.
- Personality Disorders: Particularly in borderline personality disorder and antisocial personality disorder, substance abuse is prevalent. It can be a part of harmful patterns of thinking and behavior that are characteristic of these disorders.
Each of these conditions can contribute to the onset of substance use, or vice versa, and they often make each other worse, leading to a cycle that can be hard to break without targeted treatment strategies that address both issues simultaneously.
How Does Alcohol Affect Mental Health?
 Alcohol can have significant and multifaceted effects on mental health, influencing mood, behavior, and brain function. The relationship between alcohol consumption and mental health is complex and can vary depending on factors like the amount and frequency of alcohol use, individual health status, and genetic predispositions. Here’s a look at how alcohol affects mental health:
Alcohol can have significant and multifaceted effects on mental health, influencing mood, behavior, and brain function. The relationship between alcohol consumption and mental health is complex and can vary depending on factors like the amount and frequency of alcohol use, individual health status, and genetic predispositions. Here’s a look at how alcohol affects mental health:
- Mood Fluctuations
Alcohol can initially produce feelings of relaxation and euphoria, but these effects are temporary. As alcohol levels in the blood drop, negative emotional responses can occur, such as irritability, anxiety, or sadness. Chronic alcohol use can lead to more severe mood swings and emotional instability.
- Exacerbation of Mental Health Disorders
Alcohol can worsen existing mental health conditions. For individuals with disorders like depression, anxiety, and bipolar disorder, alcohol can intensify symptoms and make them more difficult to manage. It may also interfere with the effectiveness of psychiatric medications.
- Impairment in Brain Function
Alcohol affects the brain’s neurotransmitters. These chemicals transmit signals throughout the brain and body that control thought processes, behavior, and emotion. Disruptions in neurotransmitter function due to alcohol use can result in cognitive impairments, memory loss, and reduced decision-making ability.
- Sleep Disturbances
Although some people use alcohol to help them fall asleep, it significantly impairs sleep quality and architecture. Alcohol disrupts the sleep cycle, particularly the REM stage of sleep. It is important for emotional and cognitive function. Poor sleep can contribute to a range of mental health issues, including increased stress, cognitive problems, and mood disturbances.
- Social and Behavioral Problems
Alcohol can lead to behaviors that strain personal relationships, leading to social isolation, which is a significant risk factor for mental health issues. It can also increase impulsivity, reduce inhibitions, and impair judgment, leading to poor decision-making and risky behaviors.
- Dependence and Withdrawal
Developing an alcohol dependence can have profound mental health implications. Withdrawal from alcohol can be dangerous and includes symptoms such as anxiety, depression, irritability, and severe cognitive and mood disturbances.
Given these impacts, it’s crucial for individuals experiencing mental health issues to consider the role that alcohol may play in their mental well-being and seek appropriate help.
What Are The Risks Of Mental Health And Substance Abuse?
The combination of mental health disorders and substance abuse poses several significant risks and challenges.
Risks Factors
Here are some of the key risks:
Worsening Mental Health
Substance abuse can intensify the symptoms of mental health disorders. For instance, alcohol and drugs can increase feelings of sadness or anxiety, lead to mood swings, and make depressive episodes more frequent and severe. This can make mental health conditions harder to treat and manage.
Increased Risk of Suicide
Both substance abuse and mental health disorders are independently associated with a higher risk of suicidal thoughts and behaviors. When combined, this risk can be significantly amplified.
Physical Health Problems
 Substance abuse can lead to a range of physical health issues, including liver damage, heart disease, neurological damage, and an increased risk of accidents or injuries. These conditions are often compounded by mental health disorders. It can also manifest physically as psychosomatic symptoms like headaches and gastrointestinal problems.
Substance abuse can lead to a range of physical health issues, including liver damage, heart disease, neurological damage, and an increased risk of accidents or injuries. These conditions are often compounded by mental health disorders. It can also manifest physically as psychosomatic symptoms like headaches and gastrointestinal problems.
Impaired Judgment and Risky Behaviors
Substance abuse impairs judgment and increases impulsivity, which can lead to risky behaviors such as unsafe sex, driving under the influence, or engaging in illegal activities. These behaviors can have profound legal, social, and health consequences.
Economic and Employment Challenges
Maintaining steady employment can be difficult for individuals grappling with mental health and substance use disorders. This can lead to financial instability, poverty, and further social isolation.
Increased Risk of Homelessness
The severe impacts on social relationships, employment, and economic stability can lead to homelessness, a significant risk for those with untreated dual diagnosis.
Treatment Challenges
Co-occurring mental health and substance abuse disorders complicate the diagnosis and treatment process. Each disorder can mask or mimic the symptoms of the other, leading to misdiagnosis or incomplete treatment strategies. Additionally, compliance with treatment can be more challenging due to the complex nature of these co-occurring disorders.
Higher Rates of Hospitalization and Legal Issues
Individuals with dual diagnosis are more likely to require emergency medical care, repeat hospitalizations, and have more legal issues compared to those who do not have co-occurring disorders.
Given these risks, it is crucial that treatment for individuals with dual diagnosis is comprehensive and addresses both the mental health disorder and the substance abuse issue in an integrated approach. This often involves a combination of medication, therapy, lifestyle changes, and support systems.
How To Manage Mental Health And Substance Abuse?
 Managing co-occurring mental health and substance abuse disorders requires a comprehensive and integrated approach that addresses both issues simultaneously. Here are key strategies to help:
Managing co-occurring mental health and substance abuse disorders requires a comprehensive and integrated approach that addresses both issues simultaneously. Here are key strategies to help:
1. Integrated Treatment
Integrated treatment programs are crucial as they offer services for both mental health disorders and substance abuse at the same time. These programs typically involve a combination of the following therapies:
- Psychotherapy: Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and other forms of therapy can help individuals understand the behaviors and thought patterns that lead to substance use and develop strategies to cope with mental health symptoms.
- Medication Management: Medications may be used to treat mental health disorders and, in some cases, to manage withdrawal symptoms or prevent relapse in substance use. A healthcare professional must closely monitor medication management.
- Group Therapy and Support Groups: These provide peer support and enable individuals to share experiences, learn from others, and develop social skills in a supportive environment.
2. Detoxification
The first step in treatment for substance abuse is often detoxification, which is the process of allowing the body to remove the drugs in it. Medical supervision during detox can help manage withdrawal symptoms safely and effectively.
3. Relapse Prevention
Relapse prevention strategies are vital components of treatment and recovery. These strategies include education about triggers, ongoing support, and techniques to manage stress and avoid relapse. Continuous engagement in recovery activities is crucial.
4. Lifestyle Changes
Adopting a healthy lifestyle can significantly aid recovery by improving overall physical and mental health. Important changes include:
- Regular Exercise: Physical activity can reduce stress, depression, and anxiety.
- Nutritious Diet: Proper nutrition supports brain function and overall health.
- Adequate Sleep: Sleep is crucial for emotional and physical healing.
5. Social Support
Building and maintaining a supportive social network is essential. Family therapy, coupled with support from friends who encourage sobriety and mental health management, can provide the encouragement needed to maintain recovery.
6. Educational Programs
Education about both substance abuse and mental health conditions can empower individuals to participate actively in their recovery process. Understanding the challenges and how they interrelate can help in coping with them effectively.
7. Developing Coping Skills
Skills such as stress management, emotion regulation, and conflict resolution are vital. These skills help individuals handle life’s challenges without resorting to substance use.
Proper management of dual diagnosis is complex and demands a personalized approach. Recovery is a journey, and while setbacks can occur, the right support and strategies can make long-term recovery achievable.
Conclusion
In conclusion, understanding the complex relationship between mental health and substance abuse is crucial for effective treatment and recovery. Managing these co-occurring disorders requires a comprehensive approach that includes integrated treatment programs, support from loved ones, lifestyle changes, and continuous learning and self-care.
By embracing a holistic treatment plan that addresses both mental health and substance use simultaneously, individuals can navigate the path to recovery more smoothly and sustainably. Remember, recovery is a journey that involves patience, perseverance, and the support of a compassionate community.