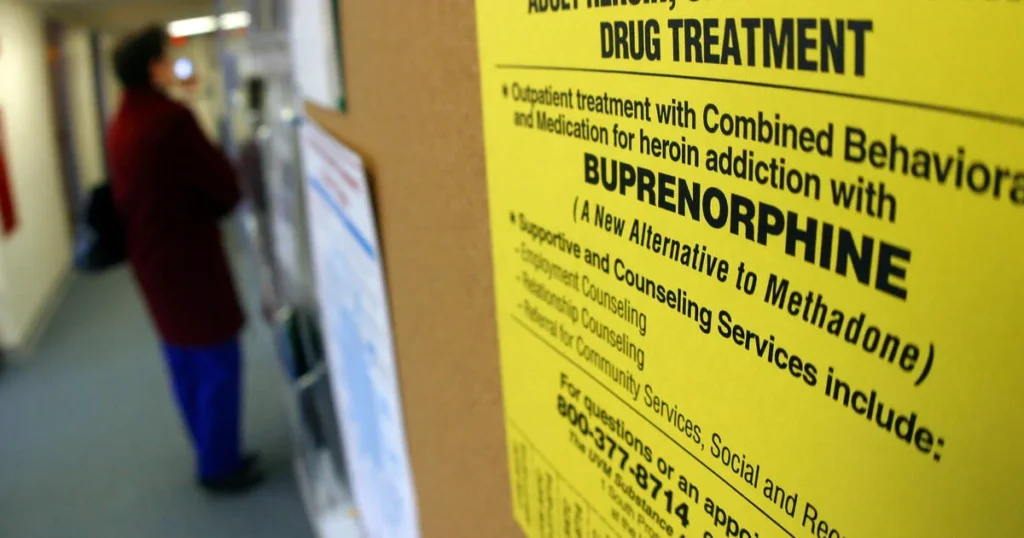
Are you or someone close to you considering Buprenorphine for opioid addiction treatment, or perhaps already using it? While it’s renowned for its effectiveness in easing the recovery process, there’s a side to it that needs careful consideration—the risk of addiction to the medication itself.
In this blog, we’re going to unravel the layers of Buprenorphine, from what it is and how it helps fight opioid addiction to the signs of its own addictive potential and the side effects it may bring. We’ll also explore the essential treatment options available if addiction occurs. Whether you’re starting treatment or are in the midst of it, understanding these aspects can empower you to make informed decisions and navigate your recovery journey safely. Let’s dive into the world of Buprenorphine together.
Contents
What is Buprenorphine?
 Buprenorphine is a medication that plays a crucial role in the treatment of opioid addiction. Classified as a partial opioid agonist, it has unique properties that make it a valuable tool for managing dependence on more potent opioids like heroin or prescription painkillers.
Buprenorphine is a medication that plays a crucial role in the treatment of opioid addiction. Classified as a partial opioid agonist, it has unique properties that make it a valuable tool for managing dependence on more potent opioids like heroin or prescription painkillers.
Classification and Action:
- Partial Opioid Agonist: Unlike full opioid agonists that fully activate the opioid receptors in the brain, Buprenorphine binds to these receptors but activates them only partially. This property helps reduce cravings and withdrawal symptoms without producing the intense high or dangerous side effects associated with stronger opioids.
Function in the Body:
- Reduction of Withdrawal Symptoms: By partially activating opioid receptors, Buprenorphine helps alleviate the symptoms of opioid withdrawal, which can include nausea, vomiting, diarrhea, and muscle pain.
- Ceiling Effect: Buprenorphine’s effects plateau at a moderate dose, meaning that there is a limit to its euphoric effects, which greatly reduces its abuse potential compared to full agonists.
Buprenorphine’s mechanism of action and its ability to limit withdrawal symptoms while curbing the potential for misuse make it a cornerstone in the modern treatment of opioid addiction. Its use allows individuals to manage withdrawal more comfortably and focus on long-term recovery strategies.
How Buprenorphine Is Used in Addiction Treatment
 Buprenorphine plays a pivotal role in the treatment of opioid addiction by providing a safer, more manageable approach to detoxification and long-term management of dependency. Here’s how it is effectively used in addiction treatment settings:
Buprenorphine plays a pivotal role in the treatment of opioid addiction by providing a safer, more manageable approach to detoxification and long-term management of dependency. Here’s how it is effectively used in addiction treatment settings:
Reduction of Cravings and Withdrawal Symptoms:
- Buprenorphine significantly reduces cravings for stronger opioids.
- It also alleviates withdrawal symptoms, which are often a major hurdle in the recovery process.
Use in Medication-Assisted Treatment (MAT):
- In MAT, Buprenorphine is used not just as a standalone treatment but as part of a comprehensive care plan that includes counseling and behavioral therapies.
- Its ceiling effect reduces the risk of misuse, overdose, and side effects associated with full opioid agonists.
The use of Buprenorphine in addiction treatment represents a significant advancement in managing opioid dependency. Its effectiveness in reducing opioid use, managing withdrawal symptoms, and its flexibility in administration make it an invaluable tool in the fight against opioid addiction.
Potential Side Effects of Buprenorphine
Buprenorphine, while effective in the treatment of opioid addiction, carries potential side effects that can impact both the health and daily activities of individuals using it. Here’s an overview of the common and serious side effects associated with Buprenorphine use:
Common Side Effects:
- Nausea and Vomiting
- Headaches
- Drowsiness and Dizziness
- Constipation
- Sweating
Serious Side Effects:
- Respiratory Depression
- Dependency and Withdrawal
- Liver Damage
- Allergic Reactions
Impact on Daily Life
The side effects of Buprenorphine can significantly affect an individual’s quality of life and ability to function normally. Drowsiness and dizziness can impair one’s ability to work or drive safely, while gastrointestinal side effects like nausea and constipation can reduce appetite and overall comfort. Understanding these potential side effects is crucial for users to manage them effectively and maintain their daily routines.
Individuals taking Buprenorphine should monitor for these side effects and consult with healthcare providers for any symptoms that persist or cause significant discomfort, ensuring adjustments can be made to their treatment plan accordingly.
Impact on Health and Well-being
 Addiction to Buprenorphine can have profound effects on an individual’s health and overall well-being.
Addiction to Buprenorphine can have profound effects on an individual’s health and overall well-being.
Physical Health Consequences:
- Respiratory Issues
- Liver Damage
- Gastrointestinal Problems
- Neurological Effects
Mental Health Consequences:
- Dependency and Withdrawal
- Altered Brain Chemistry
- Social Isolation
The impact of Buprenorphine addiction is comprehensive, affecting all areas of an individual’s life. It’s important for those experiencing this addiction or those observing it in others to seek help promptly.
Treatment Options for Buprenorphine Addiction
Managing Buprenorphine addiction requires a comprehensive treatment approach that addresses both the physiological and psychological aspects of the addiction. Here are the key strategies commonly employed to treat Buprenorphine addiction effectively:
Detoxification
- Medically Supervised Detox: The first step in treating Buprenorphine addiction often involves a medically supervised detox process to safely manage withdrawal symptoms. This controlled environment ensures that the patient can detoxify from the drug with medical assistance to mitigate potential health risks.
Therapy and Counseling
- Cognitive Behavioral Therapy (CBT): This type of therapy helps individuals identify and modify negative thought patterns and behaviors related to their addiction. CBT is effective in addressing the underlying psychological triggers of substance abuse and developing coping strategies to prevent relapse.
- Individual Counseling: One-on-one sessions with a therapist provide a safe space to explore personal issues contributing to the addiction and work through emotional and psychological challenges.
- Group Therapy: Participating in group sessions allows individuals to share experiences and gain support from others who are facing similar struggles. This can enhance motivation and foster a supportive community environment.
Medication-Assisted Treatment (MAT)
- Pharmacotherapy: Depending on the individual’s needs, other medications may be prescribed to ease withdrawal symptoms, reduce cravings, or treat concurrent mental health disorders. Medications like Naltrexone can be used to block the effects of opioids and help maintain sobriety.
- Continued Medication Management: Regular monitoring and adjustment of prescribed medications help manage long-term recovery and prevent relapse.
Support Groups
- 12-Step Programs and Peer Support Groups: Programs like Narcotics Anonymous (NA) provide ongoing support and a structured approach to recovery based on the 12-step model. These groups emphasize peer support and accountability, which are crucial for sustained recovery.
Holistic Approaches
- Lifestyle Changes: Incorporating healthy lifestyle habits such as regular exercise, proper nutrition, and adequate sleep can improve overall well-being and support recovery.
- Mindfulness and Stress Reduction Techniques: Practices like meditation, yoga, and mindfulness can help reduce stress, improve mental clarity, and enhance emotional resilience.
Effective treatment of Buprenorphine addiction involves a personalized approach that combines medical interventions with psychological support. By accessing these comprehensive treatment options, individuals struggling with Buprenorphine addiction can achieve recovery and regain control over their lives.

 Buprenorphine is prescribed to manage opioid addiction, but it can also lead to dependency if misused. Recognizing the signs of Buprenorphine addiction is crucial for addressing this issue early. Here are both behavioral changes and physical symptoms that may indicate someone is developing an addiction to Buprenorphine:
Buprenorphine is prescribed to manage opioid addiction, but it can also lead to dependency if misused. Recognizing the signs of Buprenorphine addiction is crucial for addressing this issue early. Here are both behavioral changes and physical symptoms that may indicate someone is developing an addiction to Buprenorphine: